Abstract
Introduction:
The diagnostic criteria for polycythemia vera (PV) has recently been updated by the World Health Organization (WHO). The criterion for erythrocytosis has been modified downwards: hemoglobin (hb)> 16.5 g/dL or hematocrit (hto)> 49% in men and hb> 16 g/dL or hto> 48% in women. This reduction increases the potential number of patients that would be test for JAK2 V617F mutation if PV is suspected. The V617F mutation in the JAK2 gene is present in 95% of cases of PV. It is estimated that the prevalence of this mutation in the general population is around 0.2%. Our aims are to determine the prevalence of JAK2 V617F in individuals with erythrocytosis according to WHO2016 criteria and to find prognostic factors that could help to identify patients with PV.
Methods:
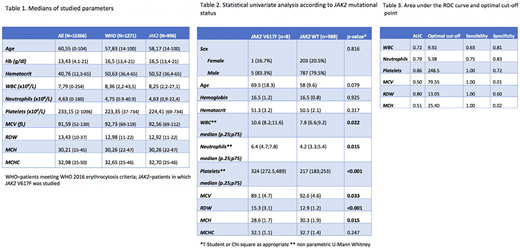
We prospectively studied all hemograms performed in our laboratory during 7 nonconsecutive days. Variables studied were hb, hto, leukocytes, neutrophils, platelets, MCV, MCH, MCHC and RDW. JAK2 V617F mutation was studied in all males that had hb> 16.5 g/dl or hto> 49% or females that had hb> 16 g/dl or hto> 48%. JAK2 V617F mutation was studied by PCR assay in which an amplification control fragment and the JAK2 mutant allele were simultaneously amplified. All positive samples were confirmed by quantitative real-time PCR in a reference laboratory. Positive results were considered when the JAK2 V617F allele ratio was ≥ 0.7.
The variables collected were correlated with the result of the JAK2 test in a univariate way. The T-Student test was used for the quantitative variables and the Chi-square test for the categorical variables. For the cell count variables, the Mann-Whitney U test was used.
Results:
A total of 15366 HG were analyzed. 1271 (8.3%) met the inclusion criteria for erythrocytosis. JAK2 V617F was performed on 1001 samples (270 samples were not suitable for the PCR assay due to low quality). Twelve samples (1.2%) were positive for JAK2 V617F mutation. However, 5 samples were excluded due to a known diagnosis of myeloproliferative neoplasm. Therefore, finally prevalence of JAK2 V617 mutation in 996 patients that met WHO erythrocytosis criteria was 0.8% (8/996). Medians for all parameter studied for each group are shown in table 1. In order to find out parameters that could increase the incidence probabilities to identify patients with JAK2 V617F we performed an univariate analysis of the variables included, according to JAK2 mutational status. We found that patients with JAK2 V617F had higher levels of leukocytes, neutrophils, platelets and RDW than patients with negative JAK2 (p <0.001), while the levels of MCV (p = 0.033) and MCH (p = 0.015) were lower in patients with JAK2 V617F (table 2). For the variables that have been statistically significant, the area under the ROC curve (AUC) and the optimal cut-off point that maximizes sensitivity and specificity were calculated (Youden index). Of interest, neutrophils, platelets and RDW show high AUC (≥ 0.79), with high sensitivity and specificity (table 3). Finally, in order to find out the potential interest of these findings, we studied medical records of the 8 patients with JAK2 V617F mutations, finding that 4 patients (50%) had previously suffered a vascular event.
Conclusion:
The prevalence of JAK2 V617F mutation in subjects with elevated Hb or hto according to WHO2016 criteria is increased with respect to that of the general population.
Among this group of subjects, those with JAK2 V617F show significantly different levels of leukocytes, neutrophils, platelets, MCV, CMH and RDW. Interestingly, neutrophils, platelets and RDW show high sensitivity and specificity. Therefore, it is necessary to explore combinations of these parameters and their optimal cut-off points to elaborate efficient strategies for an early diagnostic approach.
Martinez Lopez:Bristol Myers Squibb: Research Funding, Speakers Bureau; Novartis: Research Funding, Speakers Bureau; Celgene: Research Funding, Speakers Bureau; Janssen: Research Funding, Speakers Bureau. García Gutiérrez:Novartis: Honoraria, Research Funding; BMS: Honoraria, Research Funding; Pfizer: Honoraria, Research Funding; Incyte: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal